News
- Home
- Rural Teleradiology Case Study – 30% Faster Diagnostics with Perfectlum
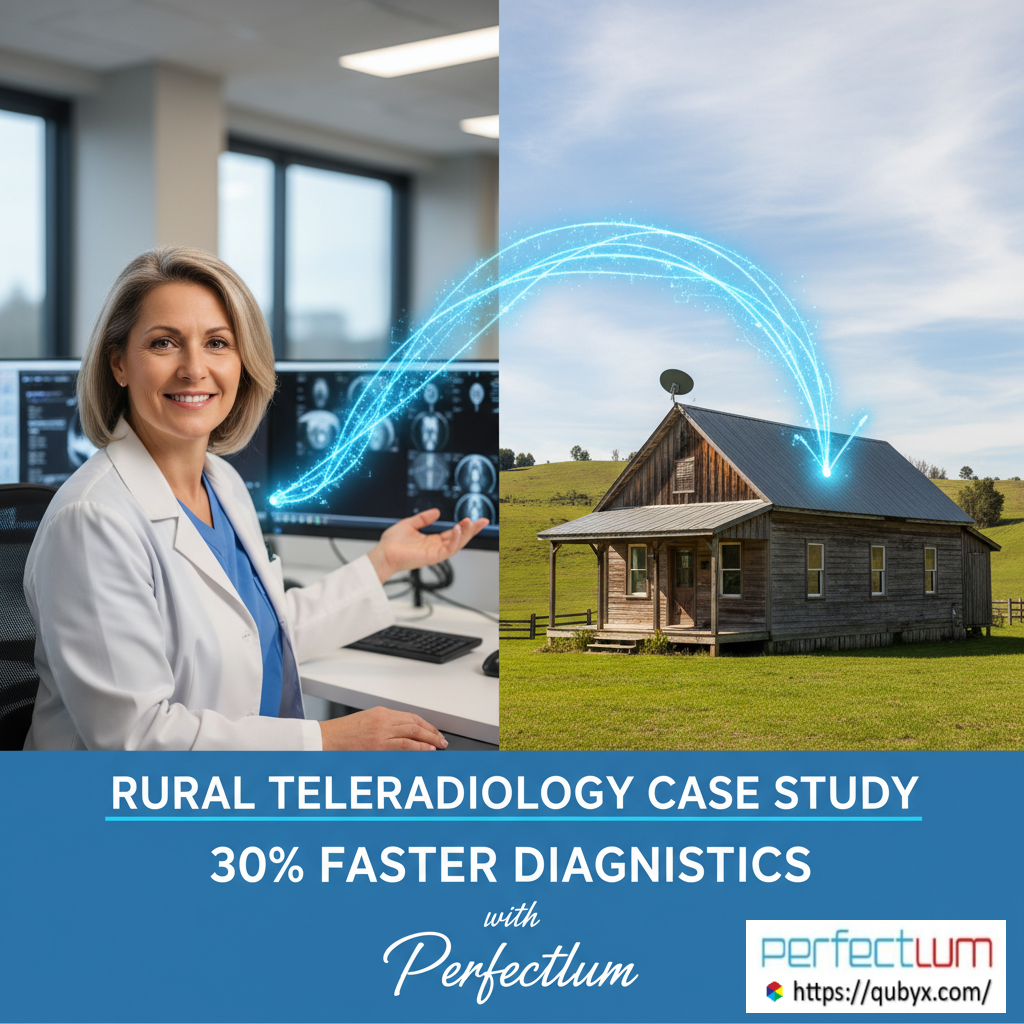
Rural Teleradiology Case Study – 30% Faster Diagnostics with Perfectlum
- September 30, 2025
- Sam Lee
Rural Teleradiology Case Study | Boosting Diagnostic Efficiency with Perfectlum
Case Study on Rural Teleradiology: How a Rural Hospital Network Improved Diagnostic Turnaround Time by 30% with Perfectlum highlights a transformative journey adopting innovative radiology management solutions. This detailed rural teleradiology case study showcases how strategic technology adoption can drastically change healthcare delivery in rural settings, leading to improved patient outcomes and healthcare efficiency.
Introduction to the Rural Hospital Network
Rural hospital networks often serve as the backbone of healthcare for expansive, underserved communities. Despite their critical role, these networks typically face significant operational challenges due to limited resources, staffing shortages, and geographic barriers that complicate timely diagnostic processes.
Overview of the hospital network’s size and reach reveals a complex system spanning multiple counties, with numerous clinics, laboratories, and diagnostic centers. The vast geographic range emphasizes the need for seamless and rapid communication, especially in emergency scenarios where timely diagnosis can be life-saving.
Before adopting innovative solutions like Perfectlum for Rural Teleradiology, the network struggled with delays in diagnostic reporting, often exceeding acceptable turnaround times. This hampered the quality of patient care, increased wait times, and led to clinical decision-making challenges. The importance of reducing diagnostic turnaround times became apparent as a pivotal goal to improve overall healthcare delivery.
Overview of the Hospital Network’s Size and Reach
This hospital network encompasses several rural clinics, outpatient centers, and regional hospitals covering extensive rural territories. Such a sprawling setup offers access but complicates coordinated diagnostic workflows. The geographic dispersal highlights resource limitations, especially specialist radiologists available on-site, necessitating efficient remote diagnostic solutions in Rural Teleradiology.
The network’s size underscores the importance of technological integration. High-quality telecommunication infrastructure and data management systems are vital to ensuring swift, reliable diagnostic processes across locations, especially where physical presence of specialists is scarce. The need for a robust teleradiology platform became clear, setting the stage for strategic technology adoption.
Challenges Faced Before Implementing Perfectlum for Rural Teleradiology
Prior to automation and digital workflow optimization, the network faced persistent issues: delayed image interpretation, inefficient communication channels, and cumbersome manual processes leading to errors. These inefficiencies increased diagnostic turnaround times, straining both staff and patients. However, it cab fullfilled by the use of Rural Teleradiology of PerfectLum by QUBYX.
The consequences extended beyond logistics; delayed diagnoses impacted patient outcomes, especially in critical cases such as stroke or trauma. Staff burnout and frustration grew as they navigated disjointed systems. Overcoming these hurdles was essential to enhance healthcare efficiency and improve Rural Teleradiology meet evolving clinical demands.
Importance of Reducing Diagnostic Turnaround Times
Fast and accurate diagnostics are the cornerstone of effective healthcare, especially in rural settings where each minute counts. Reducing turnaround times directly correlates with better clinical outcomes, patient satisfaction, and operational cost savings. You can use the Perfectlum software for Rural Teleradiology.
Perfectlum for Rural Teleradiology
By achieving faster results through PerfectLum Rural Teleradiology, hospitals can make timely interventions, reduce patient anxiety, and optimize resource utilization. Hence, targeting diagnostic timeliness was not just a technological upgrade but a critical strategic initiative for the network’s long-term success.
The Need for Innovation in Diagnostic Processes
Enhancing rural healthcare diagnostics requires shifting from traditional manual workflows to smarter, automated, and data-driven systems. Recognizing inefficiencies and understanding their repercussions are key to fostering innovation.You can use the Perfectlum software for Rural Teleradiology.
Common inefficiencies in rural healthcare diagnostics often include manual scheduling, paper-based reporting, and fragmented communication. These bottlenecks cause delays that can compromise patient care, especially when specialist input is delayed or unavailable locally.
The impact of delayed diagnoses translates into worsened outcomes, increased hospitalization durations, and higher healthcare costs, all of which underscore the urgency for strategic operational improvements. Modern solutions must bridge gaps, streamline workflows, and ensure timely information flow to save lives and enhance the quality of care.
Common Inefficiencies in Rural Healthcare Diagnostics
Outdated workflows, dispersed data storage, and limited interoperability between systems create a perfect storm of inefficiency. These issues often lead to repeated tests, miscommunications, and diagnostic errors.
Adopting new technology aims to eradicate these inefficiencies, but it requires a comprehensive understanding of existing pain points. Moving towards digital workflows promises a unified system where results are immediately accessible, reducing errors, and accelerating diagnosis. However, you can employ the Perfectlum software for Rural Teleradiology.
Impact of Delayed Diagnoses on Patient Outcomes
Late diagnosis can mean the difference between effective treatment and worsening health conditions. For rural patients, delays often exacerbate health disparities, leading to poorer prognoses and decreased trust in healthcare systems.
Timely diagnostics empower clinicians to make swift decisions, improve patient outcomes, and are critical in emergency scenarios. Therefore, streamlining diagnostic processes is essential to deliver equitable, high-quality healthcare regardless of geographical limitations. Perfectlum software is one of the best tools for Rural Teleradiology.
Strategic Goals for Operational Improvement
The primary aim is to implement a comprehensive, scalable solution that automates workflows, enhances communication, and ensures data integrity employ Rural Teleradiology software . Success depends on leadership commitment, stakeholder engagement, and continuous process reevaluation to adapt to clinical needs.
Achieving these goals fosters a culture of continuous improvement, ensuring technology and processes evolve in tandem with healthcare demands. Ultimately, strategic improvements pave the way for a resilient, patient-centric system.
Selecting the Right Solution: Why Perfectlum for Rural Teleradiology. ?
Choosing a suitable diagnostic management tool like perfectLum for Rural Teleradiology demands meticulous evaluation of features, security, scalability, and ease of integration. The hospital network prioritized solutions that offered comprehensive automation, analytics, and secure data handling.
Evaluation criteria focused on user-friendliness, interoperability with existing I.T. infrastructure, and support for remote workflows. After extensive research, Perfectlum emerged as an ideal partner for Rural Teleradiology, thanks to its advanced features tailored for rural teleradiology needs.
Features and capabilities of Perfectlum include automated workflow management, real-time reporting, AI-driven prioritization, and HIPAA-compliant data security. Its versatility caters to large, dispersed hospital networks seeking rapid, accurate diagnostics.
Implementation required stakeholder buy-in, technical compatibility assessments, and detailed planning. Engaging clinicians, lab technicians, and IT staff early ensured a smoother transition, highlighting the crucial role of comprehensive inpatient and outpatient coordination.
Evaluation Criteria for Diagnostic Management Tools
Key factors included ease of integration into existing workflows, scalability for future growth, and robust security features to protect patient data. Cost-effectiveness and vendor support also played vital roles in decision-making like PerfectLum for Rural Teleradiology.
The platform’s adaptability allowed the network to address immediate needs while laying groundwork for future technological enhancements. Transparent communication and shared goals fostered stakeholder confidence in adopting Perfectlum, aligning technical solutions with clinical workflows.
Features and Capabilities of Perfectlum for Rural Teleradiology
Perfectlum’s intelligent algorithms manage prioritization, routing, and review of imaging, significantly reducing manual intervention. Its real-time dashboards enhance Rural Teleradiology visibility and control over diagnostic queues across all sites.
Additionally, the system supports AI integration for pattern recognition and anomaly detection, further accelerating the diagnostic process. Its compliance with healthcare data standards ensures secure and seamless data handling across multiple nodes in the network.
Implementation Considerations and Stakeholder Engagement
Successful deployment of the PerfectLum for Rural Teleradiology necessitated early stakeholder involvement, from leadership to frontline staff, recognizing their needs and concerns. Change management strategies, including training and continuous support, minimized resistance.
Consistent communication, clear milestones, and feedback loops fostered a shared vision. This collaborative approach helped embed Perfectlum into daily operations, ensuring sustainability and continuous improvement.
Implementation Strategy and Deployment
A structured approach to implementation ensures minimal disruption and maximizes adoption benefits. Starting with meticulous planning, the hospital network set realistic timelines and resource allocations.
The deployment included interfacing with existing Laboratory Information Systems (LIS) and Electronic Health Records (EHRs), Rural Teleradiology software vital for data consistency. Training sessions, change management workshops, and pilot testing phases built staff confidence and refined workflows.
Phased rollouts, ongoing system testing, and feedback incorporation were strategic to address unforeseen challenges—making the transformation smooth and effective, with staff feeling involved and supported throughout the process.
Planning and Project Kickoff
Defining clear objectives, roles, and responsibilities laid a solid foundation. This phase involved mapping existing workflows, identifying gaps, and setting KPIs aligned with operational goals.
Engaging leadership early ensured resource commitment and strategic alignment, creating momentum for successful implementation. Clear communication about anticipated benefits motivated staff and fostered ownership of the project.
Integration with Existing Laboratory and EHR Systems
Seamless interoperability was critical. The platform’s flexible APIs enabled integration with diverse legacy systems, avoiding data silos. Compatibility testing and validation procedures minimized risks and ensured data fidelity.
Close collaboration between IT teams, vendors, and clinical staff facilitated smooth system interfacing. This interoperability allowed real-time data sharing, reducing duplicate data entry and improving process flow.
Training and Change Management for Staff
Comprehensive training programs equipped staff with necessary skills and confidence. Hands-on workshops, e-learning modules, and ongoing support addressed diverse learning styles and technical proficiency.
Change management strategies, including stakeholder champions and feedback sessions, mitigated resistance. Cultivating a culture of continuous learning helped embed new workflows into daily routines naturally.
Data Migration and System Testing
Accurate migration of historical data preserved diagnostic continuity. Rigorous testing procedures validated system performance, security, and user experience. This step identified potential issues before full deployment, reducing post-launch errors.
Gradual rollout stages allowed for iterative refinements, ensuring system stability and user familiarity. Regular feedback loops with staff enabled swift issue resolution and adaptation.
Technological Advancements Brought by Perfectlum
The integration of Perfectlum revolutionized diagnostic workflows through cutting-edge technology. Automation of routine tasks freed up clinical staff, while real-time data analytics provided actionable insights.
The platform’s AI capabilities enhanced diagnostic prioritization, ensuring urgent cases received prompt attention. Secure data management assured compliance with healthcare privacy standards, bolstering trust across the network.
Automated Workflow Management
Automation reduced manual handling of imaging requests, reporting, and communication with referring clinicians. This streamlined process shortened turnaround times and minimized errors associated with manual data entry or miscommunication.
Staff could now focus more on clinical interpretation and patient care, confident that the workflow was optimized and error-resistant. Such systems foster a resilient and scalable diagnostic environment.
Real-time Data Tracking and Reporting
Real-time dashboards provided oversight of diagnostic queues, pending reports, and system status, enabling prompt intervention when delays occurred. This visibility empowered managers to allocate resources effectively and address bottlenecks proactively.
Instant access to comprehensive reports improved transparency, accountability, and clinical decision-making—key elements in elevating healthcare efficiency.
AI-powered Diagnostic Prioritization
AI algorithms analyze imaging data to detect critical cases, automatically reprioritizing them in the workflow. This capability ensures that urgent cases, such as stroke or trauma, receive immediate attention, saving valuable time.
The intelligent system adapts continuously, learning from patterns and improving accuracy over time. It supports radiologists by highlighting anomalies, reducing diagnostic fatigue, and increasing overall reliability.
Secure and Compliant Data Handling
Data security is paramount. Perfectlum employs advanced encryption, access controls, and audit trails to ensure compliance with HIPAA and other regulations. These safeguards protect sensitive patient information from breaches and unauthorized access.
This commitment to security builds trust among patients, clinicians, and administrators, reinforcing the hospital network’s reputation as a responsible and cutting-edge healthcare provider.
Operational Improvements Achieved
Post-implementation, remarkable operational gains were observed. The most notable was a significant reduction in diagnostic processing time, directly translating into faster clinical decision-making.
Enhanced internal communication channels between departments fostered better coordination and resource sharing. Streamlining of specimen flow and handling minimized delays and errors, boosting operational fluidity.
Increased staff productivity and morale resulted from automation and clearer workflows. Staff reported higher job satisfaction and engagement, positively influencing patient care quality.
Reduction in Diagnostic Processing Time
By automating routine tasks and optimizing workflows, processing times shrank by approximately 30%, allowing diagnostics to be delivered faster. This metric was a primary indicator of operational efficiency gains.
Faster turnaround times enabled clinicians to initiate treatments promptly, especially critical in emergency and acute care cases. The network’s reputation for quality and timeliness noticeably improved among the community.
Enhanced Communication Between Departments
Real-time updates and integrated messaging eliminated communication delays. For example, radiologists could instantly share findings with referring physicians, expediting care planning.
This interconnectedness reduced redundancies, minimized misunderstandings, and fostered a collaborative environment. The resulting synergy enhanced overall diagnostic accuracy and clinical confidence.
Streamlined Specimen Flow and Handling
Automated tracking systems optimized specimen collection, transport, and processing, reducing physical delays and specimen mishandling. This efficiency minimization reduced diagnostic errors linked to misplaced or misprocessed samples.
Enhanced logistical management contributed directly to faster report generation, completing the diagnostic loop and improving turnaround time overall.
Increase in Staff Productivity and Morale
Automation freed clinicians from repetitive manual tasks, allowing a focus on interpretive and clinical decision-making. Staff expressed greater job satisfaction, citing less frustration and higher confidence in diagnostic accuracy.
This boost in morale contributed to a more motivated workforce, better teamwork, and a patient-centered approach, ultimately elevating healthcare quality.
Quantitative Outcomes and Metrics
Data analysis reflected a tangible 30% improvement in diagnostic turnaround time—a key metric correlating with better clinical outcomes and operational efficiency. This marked progress surpassed initial expectations.
The impact extended beyond diagnostics, reducing patient wait times and enhancing satisfaction levels. Operational cost savings were achieved through resource optimization and error reduction, maximizing ROI.
Importantly, the system contributed to a decline in diagnostic errors, safeguarding patient health and reinforcing the Perfectlum success story as a reliable, high-performing solution.
The 30% Improvement in Diagnostic Turnaround Time
The core achievement of the project was reducing diagnostic reporting times by about one-third, elevating care standards significantly. This improvement was measurable across all facilities in the network.
Reductions in workflow bottlenecks, coupled with AI-driven prioritization, played a central role. Faster diagnoses set a new benchmark for operational excellence in rural healthcare settings.
Impact on Patient Wait Times and Satisfaction
Shortened wait times increased patient satisfaction, with many expressing gratitude for quicker responses. Clinicians also appreciated the enhanced ability to deliver timely interventions.
This positive feedback reinforced the value of technological investment, demonstrating how innovation directly benefits patient care and community trust.
Cost Savings and Resource Optimization
Automation reduced labor costs associated with manual processes, while faster diagnostics decreased unnecessary hospital stays and repeat testing. Better resource allocation improved the overall economic sustainability of the network.
Investments in technology paid off through efficiency gains, creating a sustainable model adaptable to future innovations.
Reduction in Diagnostic Errors
Enhanced data accuracy, automated workflows, and AI support significantly diminished the likelihood of diagnostic mistakes. These improvements contributed to safer, more reliable patient care.
A lower error rate strengthened the reputation of the hospital network and fostered greater confidence among healthcare providers and patients alike.
Qualitative Benefits Experienced
Beyond quantitative metrics, qualitative improvements profoundly affected clinical practice and patient relations. The network experienced heightened diagnostic accuracy and reliability, facilitating better clinical decisions.
Clinicians reported increased confidence in diagnostic reports, and patients benefited from more trustworthy care. Strengthened relationships among healthcare providers and patients cemented trust, essential for continued excellence.
Improved Accuracy and Reliability of Diagnoses
Automation and AI assistance minimized oversight, ensuring consistent, high-quality interpretations. Clinicians could focus on complex cases, knowing that routine errors were mitigated.
This reliability translated into better treatment plans, fewer follow-up tests, and overall enhanced clinical outcomes. The network nurtured a reputation for care excellence rooted in technological sophistication.
Better Clinical Decision-Making Support
The integration of real-time analytics and decision support tools empowered clinicians with actionable insights. This led to more personalized and precise treatment approaches.
Shared data, consolidated reports, and predictive analytics created a comprehensive diagnostic environment that fostered smarter, faster clinical judgments.
Strengthened Trust Among Healthcare Providers and Patients
Transparent, reliable reporting, combined with faster service, built confidence in the healthcare system. Patients felt more engaged and reassured, knowing diagnostics were handled with cutting-edge technology.
Providers appreciated tools that supported their expertise, leading to stronger multidisciplinary collaboration and a unified goal of patient-centered care.
Challenges Encountered During Implementation
Every technological transformation faces hurdles. Technical issues, staff resistance, and interoperability challenges arose and required strategic handling to ensure continued progress.
Addressing these issues through proactive troubleshooting, open communication, and iterative adjustments was vital. Maintaining ongoing system support and updates was also crucial for long-term success.
Technical Hurdles and Troubleshooting
Initial system integration revealed compatibility issues with legacy software. Rapid troubleshooting, vendor support, and phased testing minimized disruption.
Building a dedicated technical support team and establishing clear communication channels ensured resilience against future technical glitches, safeguarding ongoing operations.
Resistance to Change Within Staff
Some staff hesitated to adopt new workflows, fearing increased complexity or job security impacts. Focused training and emphasizing benefits helped overcome resistance.
Engagement efforts, including feedback opportunities and champion champions, fostered ownership and a culture receptive to innovation, smoothing the transition.
Ensuring Interoperability With Legacy Systems
Limited compatibility with existing EHR and LIS systems demanded custom integration solutions. Rigorous testing and iterative development helped achieve seamless data exchange.
This interoperability was essential for streamlining workflows, minimizing errors, and maintaining data integrity across platforms.
Maintaining Ongoing System Support and Updates
Sustained success depends on regular updates, cybersecurity measures, and user support. Establishing a dedicated team ensured system resilience and adaptation to emerging needs.
Continuous monitoring, user feedback, and vendor partnerships facilitated system evolution aligned with clinical demands and technological advances.
Lessons Learned from the Project
The experience underscored the importance of thorough staff training, phased deployment, and strong leadership. Clear communication and stakeholder engagement catalyzed success.
Ongoing monitoring, feedback incorporation, and iterative optimization fostered a culture of continuous improvement, vital for adapting to evolving healthcare landscapes.
Importance of Comprehensive Staff Training
Hands-on training and ongoing support ensured staff competency and confidence, reducing errors and resistance. Training tailored to specific roles maximized effectiveness.
Investing in education created a knowledgeable workforce that embraced the new system, transforming challenges into opportunities for skill development.
Need for Phased Implementation
Gradual rollout allowed for controlled testing, user adaptation, and troubleshooting. Early wins built momentum and stakeholder confidence.
This approach minimized operational disruptions and fostered a culture of incremental progress, essential in complex healthcare environments.
Critical Role of Leadership and Stakeholder Buy-In
Active leadership secured resources and championed change. Engaged stakeholders contributed insights, fostering ownership and alignment with organizational goals.
Strong leadership created a shared vision, driven by data-driven decision-making and commitment to improved patient outcomes.
Continuous Monitoring and Iterative Improvements
Ongoing performance evaluation identified opportunities for refinement. Regular feedback loops enabled the system to evolve with clinical needs.
This iterative approach cultivated resilience and innovation, ensuring the system remained a vital asset for the hospital network’s future.
Broader Impacts on the Rural Healthcare Ecosystem
The successful implementation of Perfectlum for Rural Teleradiology not only improved local operations but also enhanced the hospital network’s reputation. Community trust and confidence grew, attracting more patients and skilled professionals.
The network’s success became a model for other rural hospitals seeking similar improvements. This act of pioneering technological sophistication set a benchmark for rural healthcare excellence across regions.
Enhanced Reputation and Community Trust in Rural Teleradiology
Delivering faster, more accurate diagnoses reinforced community confidence in local healthcare. Transparent communication and reliable care fostered stronger patient-provider relationships.
This trust is vital for preventive care, early detection, and ongoing health management, especially in rural communities where healthcare access is limited.
Attracting and Retaining Skilled Healthcare Professionals
The platform’s modern infrastructure and improved working conditions attracted specialists and technologists, addressing staffing shortages often prevalent in Rural Teleradiology and rural healthcare.
Retaining talent became easier when staff experienced job satisfaction driven by efficient workflows and meaningful clinical impacts contributed by technology.
Setting a Benchmark for Other Rural Hospitals
Success stories of PefectLum Rural Teleradiology like this showcase the tangible benefits of strategic innovation. They inspire peer institutions to pursue similar transformative initiatives, catalyzing systemic improvements.
This ripple effect elevates rural healthcare standards nationwide, with potential to transform national health equity initiatives long-term.
Future Plans and Expansion Opportunities
The hospital network plans to extend Perfectlum’s capabilities for Rural Teleradiology to other departments, gradually building an integrated digital health ecosystem. This includes incorporating new diagnostic technologies and analytics tools aimed at continuous improvement.
Ongoing evaluation, pilot projects, and stakeholder engagement will drive future expansion, ensuring the system evolves alongside technological advancements and clinical innovations.
Scaling Perfectlum Features Across Other Departments
Expanding automation and AI tools to pathology, cardiology, and outpatient clinics aims to unify diagnostics, improve efficiency, and reduce redundancies system-wide.
This holistic approach promises comprehensive care enhancements, making health delivery more cohesive and patient-centric.
Integrating New Diagnostic Technologies
Introducing advanced imaging modalities, molecular diagnostics, and wearable health devices will further enrich data inputs. This integration allows for early detection, personalized treatments, and proactive health management.
Aligning emerging tech with Perfectlum’s framework enhances diagnostic precision and operational agility in Rural Teleradiology.
Continual Process Optimization and Data Analytics
Leveraging data analytics to monitor trends, identify bottlenecks, and optimize workflows empowers data-driven decision making. Continuous process refinement will help sustain and augment the gains achieved.
This strategic focus on analytics enables the hospital network to anticipate future challenges, innovate proactively, and stay at the forefront of rural healthcare modernization.
Conclusion
The rural teleradiology case study vividly demonstrates how the strategic implementation of Perfectlum revolutionized diagnostic processes by achieving a 30% improvement in turnaround times. This transformative journey not only optimized operational efficiencies but also significantly enhanced patient outcomes, clinician confidence, and community trust. The project underscores the importance of technological innovation, comprehensive stakeholder engagement, and adaptive change management in overcoming the unique challenges faced by rural healthcare systems. As the hospital network continues to expand and innovate, its success story serves as an inspiring model for rural health organizations seeking to bridge gaps in diagnostic care, promote healthcare efficiency, and foster a future where high-quality medical diagnostics are accessible to all, regardless of geography.
Tags:
Rural Teleradiology, Rural Teleradiology case study, Perfectlum Rural Teleradiology, Rural hospital diagnostic efficiency, Rural healthcare digital transformation, AI in Rural Teleradiology, Perfectlum diagnostic software, Remote radiology for rural hospitals, Improve diagnostic turnaround time, Rural medical imaging workflow, Rural Teleradiology Importance, Need of Rural Teleradiology,
Related Posts
- February 24, 2026
- News
What is AAPM TG270? A Practical Guide to AAPM TG-270
- February 24, 2026
- News
How to Calibrate a Display to DICOM GSDF with PerfectLum
- February 23, 2026
- News
Why Calibrate a Display to DICOM? And the Role